Cervical cone
Author:
Mikael Häggström [note 1]
Unless otherwise specified, the primary focus is any cervical neoplasia.
Contents
Fixation
Generally 10% neutral buffered formalin.
See also: General notes on fixation
Gross processing
- Measure length, as well as the transverse and sagittal diameter of the ectocervical surface.[1]
- Optionally, weight the sample.[1]
- Note the symmetry of the sample, and the position of the cervical canal.[1]
- Note whether the circumference is complete. If not, and the directions are indicated on the cone, determine the approximate position of the defect.[1]
- Cones excised by knife should be inked on the excision surfaces. Those excised by laser do not need inking.[1]
Selection and trimming
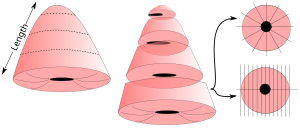
- If the cone is more than 1 cm long, take transverse slices from the top of the cone and towards the ectocervix, and stop when approximately 1 cm of the ectocervical portion of the cone remains.
- Cut the portion into radial or sagittal slices. Sagittal slices are made perpendicularly to the portion surface, and should be divided into at least the four quadrants.[note 2][1]
In cases where the cone is small and fragmented, try to orient the preparations and divide them if possible to obtain sagittal slices.[1]
See also: General notes on gross processing
Microscopic evaluation
Anatomic/Histologic location
Describe mucosa as squamous (or ectocervical), endocervical (generally mucinous and glandular) and/or transformation zone mucosa.
The anatomic level of the transformation zone varies:[2]
Type 1: Completely ectocervical (common under hormonal influence).
Type 2: Endocervical component but fully visible (common before puberty).
Type 3: Endocervical component, not fully visible (common after menopause).
Cervical dysplasia
Look for cervical dysplasia. It is mainly seen as nuclei with hyperchromasia, coarse chromatin and irregular contours.[3]
Spectrum from normal to high grade SIL.[4]
Further information: Cervical dysplasia
Radicality
Look whether there is normal epithelium on each side of all slices where neoplasia is seen, and when the epithelium is missing in any direction, consider ordering additional serial sections or step sections.
HPV changes
Also look koilocytic changes of human papillomavirus (HPV), with such cells typically displaying:
- Nuclear enlargement (two to three times normal size).
- Irregularity of the nuclear membrane contour, creating a wrinkled or raisinoid appearance.
- A darker than normal staining pattern in the nucleus, known as hyperchromasia.
- Perinuclear cytoplasmic vacuolization ("nuclear halo").
Other findings
Other common findings:
Endocervical polyp: With endocervical epithelium and glands (mucinous columnar linings), edematous stroma and clear congestion. H&E stain.[5]
Microscopy report
If a neoplasia is found, the report should include:[1]
- The histolopathological type and degree of differentiation
- Location and extent
- Radicality
|
High-grade squamous intraepithelial lesion (CIN-2), present at 3:00 to 12:00. |
Example report in a normal case:
| Cervix at transformation zone without significant histopathologic changes. Negative for neoplasia/carcinoma. |
See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ Each slice may be individually numbered.
Main page
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- ↑ International Federation for Cervical Pathology and Colposcopy (IFCPC) classification. References:
-. Transformation zone (TZ) and cervical excision types. Royal College of Pathologists of Australasia.
- Jordan, J.; Arbyn, M.; Martin-Hirsch, P.; Schenck, U.; Baldauf, J-J.; Da Silva, D.; Anttila, A.; Nieminen, P.; et al. (2008). "European guidelines for quality assurance in cervical cancer screening: recommendations for clinical management of abnormal cervical cytology, part 1 ". Cytopathology 19 (6): 342–354. doi:. ISSN 0956-5507. PMID 19040546. - ↑ Khaled J. Alkhateeb, M.B.B.S., Ziyan T. Salih, M.D.. HSIL / CIN II / CIN III. PathologyOutlines. Topic Completed: 29 March 2021. Minor changes: 9 February 2022
- ↑ Source image by Ed Uthman from Houston, TX, USA. Creative Commons Attribution 2.0 Generic (CC BY 2.0) license
- ↑ Anissa Ben Amor.. Cervical Ectropion. StatPearls, National Center for Biotechnology Information. Last Update: November 14, 2021.
- This book is distributed under the terms of the Creative Commons Attribution 4.0 International License
Image sources