Invasive melanoma of the skin
Author:
Mikael Häggström [note 1]
Melanoma of the skin generally presents as a dark skin focality.
Contents
Fixation
Generally 10% neutral buffered formalin.
See also: General notes on fixation
Gross processing
Gross examination
Note:
- Color
- Well-defined or diffuse border
- Size
- Any elevation
Tissue selection
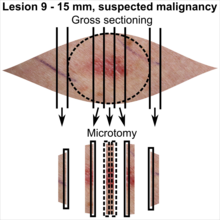
| <4 mm | 4 - 8 mm | 9 - 15 mm |
|---|---|---|

|

|
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Microscopic evaluation
Differential diagnoses
Melanoma in situ, where melanoma cells are limited to the epidermis.[2]
Further workup
In case a diagnosis of invasive melanoma of the skin can be made, the following are essentially always mandatory:
- Margins
- Depth
- Any ulceration
The following aspects are mandatory in some regions:
- Clark's level.[notes 1]
- Histopathologic type.[notes 2]
- Presence of mitoses in the intradermal component.[notes 3]
Margins
Determine if the distance to any margin is greater or lesser than 3 mm.[3] If a margin is closer, measure it at an exactness of 0.1 mm.
If margins are difficult to determine, consider immunohistochemistry with SOX10 to better visualize melanoma nests.[notes 4]
Depth and ulceration
For invasive melanoma, measure the depth and whether there is ulceration or not, so as to be able to classify the T stage (following table by AJCC, 8th edition):[4]
- TX: Primary tumor thickness cannot be assessed (such as diagnosis by curettage)
- T0: No evidence of primary tumor (such as unknown primary or completely regressed melanoma)
| Stage | T category[4] | Thickness[4] | Ulceration[4] |
|---|---|---|---|
| Stage 0 | Melanoma in situ | ||
| Stage I | T1a | Less than 0.8 mm | No |
| T1b | Less than 0.8 mm | No | |
| >0.8 to 1.0 mm | Yes | ||
| T2a | >1.0 to 2.0 mm | No | |
| Stage II | T2b | >1.0 to 2.0 mm | Yes |
| T3a | >2.0 to 4.0 mm | No | |
| T3b | >2.0 to 4.0 mm | Yes | |
| T4a | >4.0 mm | No | |
| T4b | >4.0 mm | Yes | |
Clark's level
If needing to evaluate,[notes 1] Clark's levels are:[5]
- Level 1: Melanoma confined to the epidermis (melanoma in situ)
- Level 2: Invasion into the papillary dermis
- Level 3: Invasion to the junction of the papillary and reticular dermis
- Level 4: Invasion into the reticular dermis
- Level 5: Invasion into subcutaneous tissue.
Histopathologic type
If needing to evaluate,[notes 2] the main types of invasive melanoma are:[6]
| Type | Features | Relative incidence[6][notes 5] | Photograph | Micrograph |
|---|---|---|---|---|
| Superficial spreading melanoma | Melanoma cells with nest formation along the dermo-epidermal junction. | 70% | 
|

|
| Nodular melanoma | Grows relatively more in depth than in width. | 15% - 20% | 
|
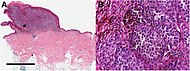
|
| Lentigo maligna melanoma | Atypical epidermal melanocytes as well as invasion into the dermis.[7] | 5% - 10% | 
|

|
| Acral lentiginous melanoma | Continuous proliferation of atypical melanocytes at the dermoepidermal junction.[8] | 7% - 10% | 
|
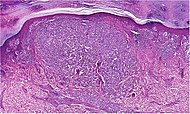
|
Other parameters
Optionally, the following parameters can be given:[9]
- histological regression, with complete or partial disappearance from areas of the dermis (and occasionally from the epidermis), which have been replaced by fibrosis, accompanied by melanophages, new blood vessels, and a variable degree of inflammation.[10]
- Further information: Evaluation of tumors
Report
Report when evaluated (as per mandatory vs. optional in Further workup above):
- >3 mm : "Clear margins" (or: "Clear margins at over __ mm")((or the exact distance thereof)).))
- <3 mm but not continuous with edge: "Close margins at __ mm at (location). [[Locations are mainly the deep edge, or the (superior/inferior/medial/lateral) radial edge.]]." Numbers are generally given at an exactness of 0.1 mm.
- Continuous with margin: "Not radically excised at (location)."
- Depth or most distant invasion of melanoma cells.[11]
- Ulceration or not
- Stage as per AJCC
- Clark's level
- Histopathologic type
- Presence of mitoses, reported only if found.[notes 3]
- Significant signs of regression
- Cytoplasmic pigmentation
- Melanoma cell shapes
Example:
|
Sun-damaged skin with central diffusely delimited proliferation of melanocytic cells having polymorphic cell nuclei, distinct nucleoli and uneven light brown pigmentation. An area of pagetoid migration is seen. There is ulceration of a smaller area. The radial margin is over 3.0 mm and the deep margin is 2.0 mm.
|
See also: General notes on reporting
Notes
- ↑ 1.0 1.1 Clark's level is not included in United States AJCC guidelines, but is mandatory for melanomas in Sweden.
-. Breslow Depth and Clark Level. Melanoma Research Alliance. Retrieved on 2020-02-13.
- . Bilaga 6. Kvalitetsbilaga för patologi (KVAST-bilaga). Regionala Cancercentrum i Samverkan, guidelines by Swedish Society of Pathology. Retrieved on 2020-02-13. - ↑ 2.0 2.1 An attempt to determine histopathologic type is mandatory for melanomas in Sweden.
- . Bilaga 6. Kvalitetsbilaga för patologi (KVAST-bilaga). Regionala Cancercentrum i Samverkan, guidelines by Swedish Society of Pathology. Retrieved on 2020-02-13. - ↑ 3.0 3.1 Presence of mitoses in the intradermal component is mandatory for melanomas in Sweden.
- . Bilaga 6. Kvalitetsbilaga för patologi (KVAST-bilaga). Regionala Cancercentrum i Samverkan, guidelines by Swedish Society of Pathology. Retrieved on 2020-02-13. - ↑ SOX10 stains cell nuclei of melanocytes.
- Miettinen, Markku; McCue, Peter A.; Sarlomo-Rikala, Maarit; Biernat, Wojciech; Czapiewski, Piotr; Kopczynski, Janusz; Thompson, Lester D.; Lasota, Jerzy; et al. (2015). "Sox10—A Marker for Not Only Schwannian and Melanocytic Neoplasms But Also Myoepithelial Cell Tumors of Soft Tissue ". The American Journal of Surgical Pathology 39 (6): 826–835. doi:. ISSN 0147-5185. - ↑ Incidence is in comparison to all melanomas.
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ The excision example shows a superficial basal cell carcinoma.
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the pointy ends to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each pointy end. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- ↑ . Melanoma in situ (stage 0). Cancer Research UK. Last reviewed: 27 Jun 2019
- ↑ Definition of "thin margin": Wolf, Y.; Balicer, R.D.; Amir, A.; Feinmesser, M.; Hauben, D.J. (2001). "The vertical dimension in the surgical treatment of cutaneous malignant melanoma – how deep is deep? ". European Journal of Plastic Surgery 24 (2): 74–77. doi:. ISSN 0930-343X.
- ↑ 4.0 4.1 4.2 4.3 Gershenwald, Jeffrey E.; Scolyer, Richard A.; Hess, Kenneth R.; Sondak, Vernon K.; Long, Georgina V.; Ross, Merrick I.; Lazar, Alexander J.; Faries, Mark B.; et al. (2017). "Melanoma staging: Evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual
". CA: A Cancer Journal for Clinicians 67 (6): 472–492. doi:. ISSN 00079235., citing
Amin MB, Edge SB, Greene FL, et al, eds. AJCC Cancer Staging Manual. 8th ed. New York: Springer International Publishing; 2017:563‐585). - ↑ . NCI Dictionary of Cancer Terms. National Cancer Institute. Retrieved on 2020-02-13.
- ↑ 6.0 6.1 [https://books.google.se/books?id=wGclDwAAQBAJ&pg=PA805 Page 805 in: Ferri, Fred (2019). Ferri's clinical advisor 2019 : 5 books in 1 . Philadelphia, PA: Elsevier. ISBN 978-0-323-52957-0. OCLC 1040695302.
- ↑ Michael Xiong; Ahmad Charifa; Chih Shan J. Chen.. Cancer, Lentigo Maligna Melanoma. StatPearls, National Center for Biotechnology Information. Last Update: May 18, 2019.
- ↑ Piliang, Melissa Peck (2009). "Acral Lentiginous Melanoma ". Surgical Pathology Clinics 2 (3): 535–541. doi:. ISSN 18759181.
- ↑ Rees, Jonathan; Viros, Amaya; Fridlyand, Jane; Bauer, Juergen; Lasithiotakis, Konstantin; Garbe, Claus; Pinkel, Daniel; Bastian, Boris C (2008). "Improving Melanoma Classification by Integrating Genetic and Morphologic Features ". PLoS Medicine 5 (6): e120. doi:. ISSN 1549-1676.
- ↑ Ribero, Simone; Gualano, Maria Rosaria; Osella-Abate, Simona; Scaioli, Giacomo; Bert, Fabrizio; Sanlorenzo, Martina; Balagna, Elena; Fierro, Maria Teresa; et al. (2015). "Association of Histologic Regression in Primary Melanoma With Sentinel Lymph Node Status ". JAMA Dermatology 151 (12): 1301. doi:. ISSN 2168-6068.
- ↑ 11.0 11.1 11.2 . An Example of a Melanoma Pathology Report. Melanoma Foundation. Retrieved on 2019-09-24.
Image sources


