Basal-cell carcinoma
Author:
Mikael Häggström [note 1]
Basal-cell carcinoma (BCC):
Contents
Fixation
Generally 10% neutral buffered formalin.
See also: General notes on fixation
Gross processing
Gross examination
Note:
- Color
- Well-defined or diffuse border
- Size
- Any elevation
Tissue selection
| <4 mm | 4 - 8 mm | 9 - 15 mm |
|---|---|---|

|

|
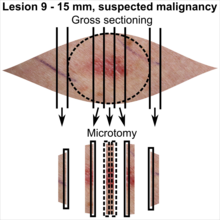
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Microscopic evaluation
Broadly consists of determining the following:
- Whether it is basal-cell carcinoma or a differential diagnosis.
- Aggressiveness pattern
- Radicality
Optionally, further subtyping of basal-cell carcinoma can be made.
Characteristics
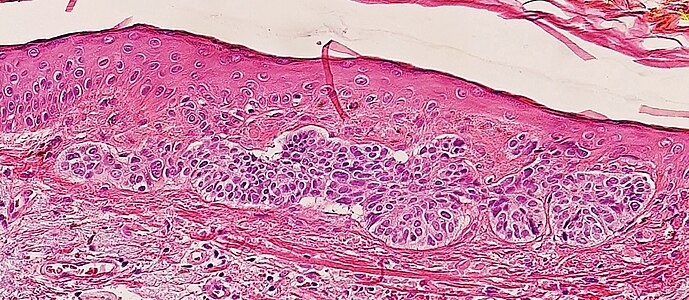
Nests of cells appearing similar to epidermal basal cells, and are usually well differentiated.[2]

In uncertain cases, immunohistochemistry using BerEP4 can be used, having a high sensitivity and specificity in detecting only BCC cells.[3]
Differential diagnoses
Main histological differential diagnoses of basal cell carcinoma:
- Hair follicles
The edges of hair follicle cells may resemble palisades, but are less pronounced, and are generally more diffusely delineated compared to surroundings.
- Squamous-cell carcinoma
Squamous-cell carcinoma of the skin is generally distinguishable by for example relatively more cytoplasm, horn cyst formation and absence of palisading and cleft formations.
Yet, a high prevalence means a relatively high incidence of borderline cases. In such cases, look particularly at the surface and attempt to classify as either of the following:
Basaloid squamous-cell carcinoma, in this case showing a biplastic pattern with basaloid elements associated with both conventional dysplastic squamous surface (arrow heads) and conventional squamous cell carcinoma (arrow).[4]
In unclear cases, the most useful immunohistochemistry marker appears to be MOC-31, which essentially always stains metatypical basal-cell carcinomas but not basaloid squamous-cell carcinomas.[5] UEA-1 appears to be the second most useful marker, staining almost all basaloid squamous-cell carcinomas but only a few metatypical basal-cell carcinomas.[5]
- Others[6]
Trichoblastoma: Absence of cleft, rudimentary hair germs, papillary mesenchymal bodies.
Adenoid cystic carcinoma: Lack of basaloid cells disposed in peripheral palisades; adenoid-cystic lesion without connection to the epidermis; absence of artefactual clefts
Microcystic adnexal carcinoma: Bland keratinocytes, keratin cysts, ductal differentiation. BerEp4- (in 60% of cases)[7], CEA+, EMA+
Trichoepithelioma:[note 3] Rims of collagen bundles, calcification, follicular/sebaceous/infundibular differentiation and cut artefacts. Cytokeratin (CK)20+, p75+, Pleckstrin homology-like domain family A member 1 + (PHLDA1+), common acute lymphoblastic leukemiaantigen + (CD10+) in tumor stroma, CK 6-, Ki-67- and Androgen Rceptor- (AR-)
Merkel cell carcinoma: Cells arranged in a diffuse, trabecular and/or nested pattern, involving also the subcutis. Mouse Anti-Cytokeratin (CAM) 5.2+, CK20+, S100-, human leukocyte common antigen- ( LCA-), thyroid transcription factor 1- (TTF1-)
Aggressiveness
Aggressiveness can be classified as low-level aggressive, moderately aggressive and highly aggressive, based mainly the cohesion of cancer cells, but also upon other histopathologic subtypes:
- Low-level aggressive patterns
Nodular. Also known as "classic basal-cell carcinoma". It accounts for 50% of all BCC.[6] It typically has relatively cohesive aggregates of basaloid cells with well-defined borders, showing palisading and one or more clefts.[6] Central necrosis with eosinophilic, granular features may be also present, as well as mucin. The heavy aggregates of mucin determine a cystic structure. Calcification may be also present, especially in long-standing lesions.[6] Mitotic activity is usually not so evident, but a high mitotic rate may be present in more aggressive lesions.[6]
Fibroepitheliomatous pattern: anastomosing basaloid epithelial strands enclosing round islands of fibrous stroma[8]
- Moderately aggressive pattern
- Highly aggressive patterns
Cicatricial or morphoeic pattern: Narrow strands and nests of basaloid cells, typically with sharp edges, surrounded by dense sclerotic stroma.[9]
Radicality
Determine if there are basal-cell formations continuous with resection margins, or if they are closer or farther than 1 mm from the closest edge.[10] If closer, measure the distance.
If uncertain, immunohistochemistry with BerEP4 helps in distinguishing the BCC cells.

- Further information: Evaluation of tumors
Reporting
- Aggressiveness pattern, at least if highly aggressive.
- Radicality, mainly into either of the following:
- >1 mm (as per Radicality above): "Clear margins" (or: "Clear margins at over __ mm")((or the exact distance thereof)).))
- <1 mm but not continuous with edge: "Close margins at __ mm at (location). [[Locations are mainly the deep edge, or the (superior/inferior/medial/lateral) radial edge.]]." Numbers are generally given at an exactness of 0.1 mm.[10]
- Continuous with margin: "Not radically excised at (location)."
Optionally, subtype of basal-cell carcinoma
Example:
| (Skin excision with stratified squamous keratinized epithelium, where the dermis contains) moderately aggressive basal-cell carcinoma, not radically excised at the right margin.[note 4] |
See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ The excision example shows a superficial basal cell carcinoma.
- ↑ Desmoplastic tricoepithelioma is particularly similar to basal-cell carcinoma.
- ↑ The direction was known from needle marking.
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the pointy ends to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each pointy end. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- ↑ Robert S Bader. Which histologic findings are characteristic of basal cell carcinoma (BCC)?. Medscape. Updated: Feb 21, 2019
- ↑ 3.0 3.1 Sunjaya, Anthony Paulo; Sunjaya, Angela Felicia; Tan, Sukmawati Tansil (2017). "The Use of BEREP4 Immunohistochemistry Staining for Detection of Basal Cell Carcinoma ". Journal of Skin Cancer 2017: 1–10. doi:. ISSN 2090-2905.
- ↑ El-Mofty, SK. (2014). "Histopathologic risk factors in oral and oropharyngeal squamous cell carcinoma variants: An update with special reference to HPV-related carcinomas
". Medicina Oral Patología Oral y Cirugia Bucal: e377–e385. doi:. ISSN 16986946.
License: CC BY 2.5 - ↑ 5.0 5.1 Webb, David V.; Mentrikoski, Mark J.; Verduin, Lindsey; Brill, Louis B.; Wick, Mark R. (2015). "Basal cell carcinoma vs basaloid squamous cell carcinoma of the skin: an immunohistochemical reappraisal ". Annals of Diagnostic Pathology 19 (2): 70–75. doi:. ISSN 10929134.
- ↑ 6.0 6.1 6.2 6.3 6.4 Paolino, Giovanni; Donati, Michele; Didona, Dario; Mercuri, Santo; Cantisani, Carmen (2017). "Histology of Non-Melanoma Skin Cancers: An Update ". Biomedicines 5 (4): 71. doi:. ISSN 2227-9059.
- ↑ Inskip, Mike; Magee, Jill (2015). "Microcystic adnexal carcinoma of the cheek—a case report with dermatoscopy and dermatopathology ". Dermatology Practical & Conceptual 5 (1). doi:. ISSN 21609381.
- ↑ Yonan, Yousif; Maly, Connor; DiCaudo, David; Mangold, Aaron; Pittelkow, Mark; Swanson, David (2019). "Dermoscopic Description of Fibroepithelioma of Pinkus with Negative Network ". Dermatology Practical & Conceptual: 246–247. doi:. ISSN 2160-9381. Creative Commons Attribution License
- ↑ East, Ellen; Fullen, Douglas R.; Arps, David; Patel, Rajiv M.; Palanisamy, Nallasivam; Carskadon, Shannon; Harms, Paul W. (2016). "Morpheaform Basal Cell Carcinomas With Areas of Predominantly Single-Cell Pattern of Infiltration ". The American Journal of Dermatopathology 38 (10): 744–750. doi:. ISSN 0193-1091.
- ↑ 10.0 10.1 David Slater, Paul Barrett. Standards and datasets for reporting cancers - Dataset for histopathological reporting of primary cutaneous basal cell carcinoma. The Royal College of Pathologists. February 2019
Image sources