Difference between revisions of "Emergency pathology"
(Expanded) |
(Continued) |
||
| Line 3: | Line 3: | ||
|author2= | |author2= | ||
}} | }} | ||
| − | + | <noinclude>This article is written specifically for new pathology trainees. | |
| − | === | + | </noinclude>{{Memorization-worthy}} Information relating to emergent pathology is often not conveniently and timely looked up when needed because of the need for a fast report. |
| + | |||
| + | ==Frozen sections== | ||
| + | Even new pathology trainees may end up being the first responders to frozen sections. | ||
| + | |||
| + | ===Preparation=== | ||
| + | Prepare at least the following: | ||
[[File:Micrography with a smartphone.jpg|thumb|230px|To perform '''micrography''' with a smartphone, stabilize the smartphone over the eyepiece (preferably using both hands), and move it slowly around until most of the microscopic field is in focus.]] | [[File:Micrography with a smartphone.jpg|thumb|230px|To perform '''micrography''' with a smartphone, stabilize the smartphone over the eyepiece (preferably using both hands), and move it slowly around until most of the microscopic field is in focus.]] | ||
| − | + | *Finding out '''which senior to call for help''' if responding to a frozen section. A fairly new pathology trainee should generally not independently make a report to the referring physician without having at least consulted with a senior, and therefore the diagnostics of frozen section slides is not included in this section. In the meantime, ensure that you have a working smartphone available, and know beforehand who to contact whenever you are at risk of being responsible for a frozen section, so that you can perform '''micrography''' of the slide in case and send it to the senior if that person can not be physically present within an acceptable time. | |
| − | + | *If possible, look up pertinent '''medical histories''' of potential cases that may appear as frozen sections or other forms of intraoperative consultations. For example, surgery departments may have schedules of patients for the day that you will cover frozen sections. On such lists, types of surgeries that often come as intraoperative consultations mainly include potentially malignant skin excisions, lung excisions (larger than biopsies) and ovarian tumors. | |
| − | |||
| − | |||
| − | + | ===Suspected malignant skin excisions=== | |
| + | While most frozen sections can be predicted from schedules of the operating room and thereby be looked up beforehand, suspected malignant skin excisions often come from outside the main surgery department, even more indicating memorization of how to handle them. | ||
| + | {{Tissue selection from suspected malignant skin lesions}} | ||
| − | + | ===Other frozen sections=== | |
Although these are generally given on schedules of the operating room, any pathologist may end up suddenly covering for another one, and subsequently be presented with the frozen section case without having had the time to look it up beforehand. | Although these are generally given on schedules of the operating room, any pathologist may end up suddenly covering for another one, and subsequently be presented with the frozen section case without having had the time to look it up beforehand. | ||
| + | {{Bottom}} | ||
Revision as of 19:44, 9 December 2021
Author:
Mikael Häggström [note 1]
This article is written specifically for new pathology trainees.
Memorization-worthy:[note 2] Information relating to emergent pathology is often not conveniently and timely looked up when needed because of the need for a fast report.
Contents
Frozen sections
Even new pathology trainees may end up being the first responders to frozen sections.
Preparation
Prepare at least the following:
- Finding out which senior to call for help if responding to a frozen section. A fairly new pathology trainee should generally not independently make a report to the referring physician without having at least consulted with a senior, and therefore the diagnostics of frozen section slides is not included in this section. In the meantime, ensure that you have a working smartphone available, and know beforehand who to contact whenever you are at risk of being responsible for a frozen section, so that you can perform micrography of the slide in case and send it to the senior if that person can not be physically present within an acceptable time.
- If possible, look up pertinent medical histories of potential cases that may appear as frozen sections or other forms of intraoperative consultations. For example, surgery departments may have schedules of patients for the day that you will cover frozen sections. On such lists, types of surgeries that often come as intraoperative consultations mainly include potentially malignant skin excisions, lung excisions (larger than biopsies) and ovarian tumors.
Suspected malignant skin excisions
While most frozen sections can be predicted from schedules of the operating room and thereby be looked up beforehand, suspected malignant skin excisions often come from outside the main surgery department, even more indicating memorization of how to handle them.
Tissue selection
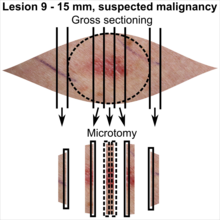
| <4 mm | 4 - 8 mm | 9 - 15 mm |
|---|---|---|

|

|
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Other frozen sections
Although these are generally given on schedules of the operating room, any pathologist may end up suddenly covering for another one, and subsequently be presented with the frozen section case without having had the time to look it up beforehand.
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ Further information on what is memorization-worthy or not: Learning pathology
- ↑ The excision example shows a superficial basal cell carcinoma.
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the pointy ends to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each pointy end. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
Image sources
