Difference between revisions of "Renal tumor"
Jump to navigation
Jump to search
(Expanded) |
(Started) |
||
| Line 8: | Line 8: | ||
==Gross processing== | ==Gross processing== | ||
| − | |||
For orientation, the ureter stump points to the inferior pole.<ref name=stora/> | For orientation, the ureter stump points to the inferior pole.<ref name=stora/> | ||
| Line 14: | Line 13: | ||
*Note the appearance of the renal surface | *Note the appearance of the renal surface | ||
*Inspect the capsule and pericapsular soft tissue, and possibly an accompanying adrenal gland | *Inspect the capsule and pericapsular soft tissue, and possibly an accompanying adrenal gland | ||
| − | *Measure dimensions (and optionally | + | *Measure kidney dimensions (and optionally weight) |
*Identify the surgical margin of the ureteral stump, renal vein and renal artery | *Identify the surgical margin of the ureteral stump, renal vein and renal artery | ||
*In cases of a bulging tumor, apply ink to the surface of pericapsular fatty tissue by the tumor. | *In cases of a bulging tumor, apply ink to the surface of pericapsular fatty tissue by the tumor. | ||
| Line 20: | Line 19: | ||
*Split the kidney in the middle, in the coronal plane. Release the fibrous capsule. Dissect the renal pelvis and calyces. Inspect the parenchyma on cut surfaces. | *Split the kidney in the middle, in the coronal plane. Release the fibrous capsule. Dissect the renal pelvis and calyces. Inspect the parenchyma on cut surfaces. | ||
:*Note and possibly measure the medullary thickness and the width of the renal pelvis | :*Note and possibly measure the medullary thickness and the width of the renal pelvis | ||
| + | :*Note the appearance of any concretions | ||
| + | *Note the location and size of the tumor, macroscopic appearance of cut surfaces, delimitation compared to surrounding structures, and relation to the fibrous capsule and perinephric tissues. If the fibrous capsule can be detached from the tumor surface, the inside of the capsule is examined where it was in contact with tumor, in order to detect any tumor overgrowth or breakthrough. | ||
| − | + | ===Slices for submission=== | |
| − | === | + | Including:<ref name=stora/> |
| + | *At least 3-4 pieces from the tumor, showing relationship to surrounding kidney tissue, renal capsule, perinephric tissues, renal pelvis, hilar adipose tissue and blood vessels. | ||
| + | *Part of the fibrous capsule if being in contact with the tumor (oriented perpendicular to the capsular surface) | ||
| + | *Margins of ureteral stump, renal vein and renal artery, and from hilus tissue (to detect possible tumor invasion of smaller blood vessels) | ||
| + | *One slice of normal kidney tissue | ||
| + | *Any detected lymph nodes in perihilar region | ||
| + | *At least one slice from any included adrenal gland. | ||
| + | *In case of cancer in the renal pelvis, at least three slices from the tumor-suspected area, including radicality slices from surrounding normal mucosa, and adjacent peripelvic fatty tissue. Take about 1 piece per cm<sup>2</sup> from other parts of the renal pelvis, as well as a piece from the surgical edge of the ureteral stump. | ||
| − | + | ==Microscopic evaluation== | |
| + | {| class="wikitable" | ||
| + | ! Renal carcinoma subtype !! Characteristic morphology<ref name="SirohiSmith2018">{{cite journal|last1=Sirohi|first1=Deepika|last2=Smith|first2=Steven C.|last3=Agarwal|first3=Neeraj|last4=Maughan|first4=Benjamin L.|title=Unclassified renal cell carcinoma: diagnostic difficulties and treatment modalities|journal=Research and Reports in Urology|volume=Volume 10|year=2018|pages=205–217|issn=2253-2447|doi=10.2147/RRU.S154932}}</ref> !! Positive immunohistochemistry<ref name="SirohiSmith2018"/> !! Image | ||
| + | |- | ||
| + | | Clear-cell RCC || Clear cells in nests or solid pattern, delicate branching fibrovascular network || Vimentin, EMA, keratin, CD 10, Pax2, RCC, CAIX (circumferential membranous) || [[File:Histopathology of renal clear cell carcinoma.jpg|190px]] | ||
| + | |- | ||
| + | | Papillary RCC I || Papillary architecture, small-to-medium-sized cells, histiocytes in fibrovascular cores || Vimentin, keratins, CK7, AMACR, RCC || [[File:Histopathology of papillary renal cell carcinoma type 1.jpg|190px]] | ||
| + | |- | ||
| + | | Papillary RCC 2 || Papillary architecture, medium to large cell, pseudostratified nuclei || Variable | ||
| + | |- | ||
| + | | Clear-cell papillary RCC || Clear cells in papillary, solid, or nested pattern, abluminal linear arrangement of nuclei || CA-IX (basolateral membranous), HMWCK | ||
| + | |- | ||
| + | | Chromophobe || Vegetable-like nuclei, raisnoid nuclei with perinuclear halos || Ksp Cadherin, CD 1 17, EMA, keratins, CK7 | ||
| + | |- | ||
| + | | Oncocytoma || Small nests of cells, uniform small nuclei || Ksp Cadherin, CD 1 17, EMA, keratins | ||
| + | |- | ||
| + | | CDC || Infiltrating high-grade adenocarcinoma centered in the medulla, desmoplastic stroma || EMA, CK7, HMWCK, Pax 2, Pax 8 | ||
| + | |- | ||
| + | | MITF-RCC || Clear and eosinophilic cells, voluminous cytoplasm, psammomatous calcifications (TFE3) | ||
| + | |- | ||
| + | | Biphasic tumors (TFEB) || HMB-45, Melan A, Cathepsin K,TFE3/TFEB | ||
| + | |- | ||
| + | | FH-deficient RCC || Variable, intracystic papillary pattern with prominent hyalinization and most frequent tubulocystic patterns || Loss of FH (deficient), 2SC | ||
| + | |- | ||
| + | | SDH-deficient RCC || Oncocytic cells with cytoplasmic vacuoles and inclusion-like spaces, neuroendocrine-like chromatin || SDHB loss (deficient) | ||
| + | |- | ||
| + | | RMC || High-grade adenocarcinoma, inflammatory, myxoid, or desmoplastic stroma, evidence of sickle cell trait/disease || INI-I loss, Oct 1/4 positive | ||
| + | |} | ||
| − | + | ==Report== | |
| − | + | The report should include:<ref name=stora/> | |
| − | + | *Total or partial nephrectomy | |
| − | + | *Tumor characteristics: | |
| − | + | *location | |
| − | + | *Size | |
| − | + | *Relationship to capsule, perinephric tissues, renal pelvis, adrenal gland and hilar blood vessels | |
| − | + | *Histological type | |
| − | + | *Degree of differentiation | |
| − | + | *Radicality | |
| − | + | *Any lymph node metastases | |
| − | + | {{Bottom}} | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | The | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Revision as of 09:41, 4 February 2020
Author:
Mikael Häggström [note 1]
Contents
Presentations
Usually total nephrectomy.[1]
Gross processing
For orientation, the ureter stump points to the inferior pole.[1]
Components:[1]
- Note the appearance of the renal surface
- Inspect the capsule and pericapsular soft tissue, and possibly an accompanying adrenal gland
- Measure kidney dimensions (and optionally weight)
- Identify the surgical margin of the ureteral stump, renal vein and renal artery
- In cases of a bulging tumor, apply ink to the surface of pericapsular fatty tissue by the tumor.
- Dissect the ureteral stump
- Split the kidney in the middle, in the coronal plane. Release the fibrous capsule. Dissect the renal pelvis and calyces. Inspect the parenchyma on cut surfaces.
- Note and possibly measure the medullary thickness and the width of the renal pelvis
- Note the appearance of any concretions
- Note the location and size of the tumor, macroscopic appearance of cut surfaces, delimitation compared to surrounding structures, and relation to the fibrous capsule and perinephric tissues. If the fibrous capsule can be detached from the tumor surface, the inside of the capsule is examined where it was in contact with tumor, in order to detect any tumor overgrowth or breakthrough.
Slices for submission
Including:[1]
- At least 3-4 pieces from the tumor, showing relationship to surrounding kidney tissue, renal capsule, perinephric tissues, renal pelvis, hilar adipose tissue and blood vessels.
- Part of the fibrous capsule if being in contact with the tumor (oriented perpendicular to the capsular surface)
- Margins of ureteral stump, renal vein and renal artery, and from hilus tissue (to detect possible tumor invasion of smaller blood vessels)
- One slice of normal kidney tissue
- Any detected lymph nodes in perihilar region
- At least one slice from any included adrenal gland.
- In case of cancer in the renal pelvis, at least three slices from the tumor-suspected area, including radicality slices from surrounding normal mucosa, and adjacent peripelvic fatty tissue. Take about 1 piece per cm2 from other parts of the renal pelvis, as well as a piece from the surgical edge of the ureteral stump.
Microscopic evaluation
| Renal carcinoma subtype | Characteristic morphology[2] | Positive immunohistochemistry[2] | Image |
|---|---|---|---|
| Clear-cell RCC | Clear cells in nests or solid pattern, delicate branching fibrovascular network | Vimentin, EMA, keratin, CD 10, Pax2, RCC, CAIX (circumferential membranous) | 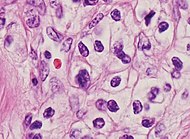
|
| Papillary RCC I | Papillary architecture, small-to-medium-sized cells, histiocytes in fibrovascular cores | Vimentin, keratins, CK7, AMACR, RCC | 
|
| Papillary RCC 2 | Papillary architecture, medium to large cell, pseudostratified nuclei | Variable | |
| Clear-cell papillary RCC | Clear cells in papillary, solid, or nested pattern, abluminal linear arrangement of nuclei | CA-IX (basolateral membranous), HMWCK | |
| Chromophobe | Vegetable-like nuclei, raisnoid nuclei with perinuclear halos | Ksp Cadherin, CD 1 17, EMA, keratins, CK7 | |
| Oncocytoma | Small nests of cells, uniform small nuclei | Ksp Cadherin, CD 1 17, EMA, keratins | |
| CDC | Infiltrating high-grade adenocarcinoma centered in the medulla, desmoplastic stroma | EMA, CK7, HMWCK, Pax 2, Pax 8 | |
| MITF-RCC | Clear and eosinophilic cells, voluminous cytoplasm, psammomatous calcifications (TFE3) | ||
| Biphasic tumors (TFEB) | HMB-45, Melan A, Cathepsin K,TFE3/TFEB | ||
| FH-deficient RCC | Variable, intracystic papillary pattern with prominent hyalinization and most frequent tubulocystic patterns | Loss of FH (deficient), 2SC | |
| SDH-deficient RCC | Oncocytic cells with cytoplasmic vacuoles and inclusion-like spaces, neuroendocrine-like chromatin | SDHB loss (deficient) | |
| RMC | High-grade adenocarcinoma, inflammatory, myxoid, or desmoplastic stroma, evidence of sickle cell trait/disease | INI-I loss, Oct 1/4 positive |
Report
The report should include:[1]
- Total or partial nephrectomy
- Tumor characteristics:
- location
- Size
- Relationship to capsule, perinephric tissues, renal pelvis, adrenal gland and hilar blood vessels
- Histological type
- Degree of differentiation
- Radicality
- Any lymph node metastases
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
Main page
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- ↑ 2.0 2.1 Sirohi, Deepika; Smith, Steven C.; Agarwal, Neeraj; Maughan, Benjamin L. (2018). "Unclassified renal cell carcinoma: diagnostic difficulties and treatment modalities ". Research and Reports in Urology Volume 10: 205–217. doi:. ISSN 2253-2447.
Image sources