Template:Overlap of squamous-cell and basal-cell carcinoma
Author:
Mikael Häggström [note 1]
Yet, a high prevalence means a relatively high incidence of borderline cases, with main forms being:
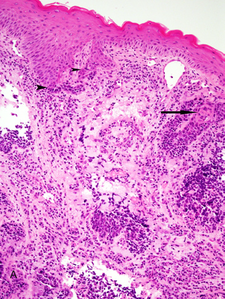
Basaloid squamous-cell carcinoma, in this case showing a biplastic pattern with conventional dysplastic squamous surface component associated with basaloid elements (arrow heads) and conventional squamous cell carcinoma intimately associated with basaloid component (arrow).[1]
In unclear cases, the most useful immunohistochemistry marker appears to be MOC-31, which essentially always stains metatypical basal-cell carcinomas but not basaloid squamous-cell carcinomas.[2] UEA-1 appears to be the second most useful marker, staining almost all basaloid squamous-cell carcinomas but only a few metatypical basal-cell carcinomas.[2]
Contents
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
Main page
References
- ↑ El-Mofty, SK. (2014). "Histopathologic risk factors in oral and oropharyngeal squamous cell carcinoma variants: An update with special reference to HPV-related carcinomas
". Medicina Oral Patología Oral y Cirugia Bucal: e377–e385. doi:. ISSN 16986946.
License: CC BY 2.5 - ↑ 2.0 2.1 Webb, David V.; Mentrikoski, Mark J.; Verduin, Lindsey; Brill, Louis B.; Wick, Mark R. (2015). "Basal cell carcinoma vs basaloid squamous cell carcinoma of the skin: an immunohistochemical reappraisal ". Annals of Diagnostic Pathology 19 (2): 70–75. doi:. ISSN 10929134.
Image sources