Ovarian tumor
Author:
Mikael Häggström [note 1]
Contents
Comprehensiveness
On this resource, the following formatting is used for comprehensiveness:
- Minimal depth
- (Moderate depth)
- ((Comprehensive))
Microscopic evaluation
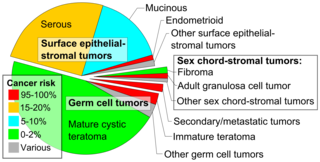
Look for the most common types of ovarian tumor:
| Type | Subtype | Relative incidence[2] | Comments | Micrograph |
|---|---|---|---|---|
| Germ cell tumor | Dermoid cyst (teratoma) | 46% | Cystic, with elements of all 3 germ layers (endoderm, mesoderm and ectoderm).[3] | |
| Immature teratoma | 2.5% | A teratoma that contains anaplastic immature elements, and is often synonymous with malignant teratoma.[4] | 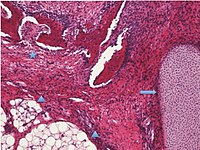
| |
| Other germ cell tumors | 3.0% | Others mainly include dysgerminoma, yolk sac tumor, struma ovarii and squamous cell carcinoma arising from a dermoid cyst, and malignant mixed germ cell tumor.[2] |
 Histopathology of yolk sac tumor with Schiller–Duval bodies.[5] | |
| Surface epithelial-stromal tumor | Serous tumor | 25% | Benign serous tumors of the right ovarian cyst are thinwalled unilocular cysts that are lined by ciliated pseudostratified cuboidal or columnar epithelium.[6] | 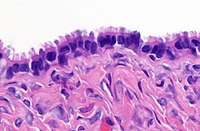
|
| Mucinous tumor | 15% | Benign mucinous tumors of the ovary consist of simple, nonstratified columnar epithelium with basally-located hyperchromatic nuclei and resemble gastric foveolar epithelium.[6] | 
| |
| Endometrioid tumor | 1% | Tubular glands, resembling endometrium.[7] | 
| |
| Other surface-epithelial tumors | 1.5% | Others include mainly malignant mixed mullerian tumor, Brenner tumor and mixed epithelial tumor.[2] | ||
| Sex cord-stromal tumor | Ovarian fibroma | 1.5% | Spindle-shaped fibroblastic cells and abundant collagen.[8] | 
|
| Adult granulosa cell tumor | 1% | Small, bland, cuboidal to polygonal cells in various patterns.[9] Grooved, coffee bean-like nuclei.[10] | 
| |
| Leydig cell tumor | <1% | 
| ||
| Other sex cord-stromal tumors | 1% | Others include mainly juvenile granulosa cell tumor, thecoma and sclerosing stromal tumor[2] | ||
| Secondary/metastatic) tumor | 2% | Usually from breast cancer, colon cancer, endometrial cancer, stomach cancer or cervical cancer.[12] | ||
An ovarian serous borderline tumor is a subgroup of borderline tumors, with up to moderate atypia.
Differential diagnosis
Mesonephric duct remnant: Small tubules lined by low columnar to cuboidal cells without cilia, and surrounded by ample smooth muscle.[13]
Bilateral tumors
In cases of a tumor in both ovaries, of presumable ovarian origin, the largest tumor is generally designated as the "primary tumor" if needed (generally as a mandatory entry in synoptic reports of malignant tumors). ((Add a comment that "The largest tumor is designated as the primary".))
Staging
Also include any peritoneal fluid sample.
Perform staging for malignant tumors, as follows:[14]
| Primary tumor (T) | ||
|---|---|---|
| TNM | FIGO | |
| TX | Primary tumor cannot be assessed | |
| T0 | No evidence of primary tumor | |
| T1 | I | Tumor confined to the ovaries or fallopian tubes |
| T1a | IA | Tumor limited to one ovary (capsule intact) or fallopian tube; no tumor on ovarian or fallopian tube surface; no malignant cells in ascites or peritoneal washings |
| T1b | IB | Tumor limited to both ovaries (capsule intact) or fallopian tubes; no tumor on ovarian or fallopian tube surface; no malignant cells in ascites or peritoneal washings |
| T1c | IC | Tumor limited to one or both ovaries or fallopian tubes with any of the following: |
| T1c1 | IC1 | Surgical spill |
| T1c2 | IC2 | Capsule ruptured before surgery or tumor on ovarian or fallopian tube surface |
| T1c3 | IC3 | Malignant cells in ascites or peritoneal washings |
| T2 | II | Tumor involves one or both ovaries or fallopian tubes with pelvic extension (below pelvic brim) or peritoneal cancer |
| T2a | IIA | Extension and/or implants on uterus and/or tube(s) and/or ovaries |
| T2b | IIB | Extension and/or implants on other pelvic tissues |
| T3 | III | Tumor involves one or both ovaries or fallopian tubes, or primary peritoneal cancer, with microscopically confirmed peritoneal metastasis outside the pelvis and/or metastases to the retroperitoneal (pelvic and/or para-aortic) lymph nodes |
| IIIA | Positive retroperitoneal lymph nodes and/or microscopic metastasis beyond pelvis | |
| IIIA1 | Positive retroperitoneal lymph nodes only (cytologically or histologically proven) | |
| IIIA1 (i) | Metastasis up to 10 mm in greatest dimension | |
| IIIA1 (ii) | Metastasis more than 10 mm in greatest dimension | |
| T3a | IIIA2 | Microscopic extrapelvic (above the pelvic brim) peritoneal involvement, with or without positive retroperitoneal lymph nodes |
| T3b | IIIB | Macroscopic peritoneal metastasis beyond pelvis up to 2 cm in greatest dimension, with or without metastasis to the retroperitoneal lymph nodes |
| T3c | IIIC | Macroscopic peritoneal metastasis beyond the pelvis >2 cm in greatest dimension including extension to liver capsule or spleen without parenchymal involvement of those organs and with or without positive retroperitoneal lymph nodes |
| Regional lymph nodes (N) | ||
|---|---|---|
| TNM | FIGO | |
| NX | Regional lymph nodes cannot be assessed | |
| N0 | No regional lymph node metastasis | |
| N0(i+) | Isolated tumor cells in regional lymph node(s) ≤0.2 mm | |
| N1 | IIIA1 | Positive (histologically confirmed) retroperitoneal lymph nodes |
| N1a | IIIAIi | Metastasis ≤10 mm in greatest dimension |
| N1b | IIIAIii | Metastasis more than 10 mm in greatest dimension |
| Distant metastasis (M) | ||
|---|---|---|
| TNM | FIGO | |
| M0 | No distant metastasis | |
| M1 | IV | Distant metastasis including cytology-positive pleural effusion; liver or splenic parenchymal involvement; extra-abdominal organ involvement including inguinal lymph nodes; transmural intestinal involvement |
| M1a | IVA | Pleural effusion with positive cytology |
| M1b | IVB | Liver or splenic parenchymal metastases; metastases to extra-abdominal organs (including inguinal lymph nodes and lymph nodes outside the abdominal cavity); transmural involvement of intestine |
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
Main page
References
- ↑ - Vaidya, SA; Kc, S; Sharma, P; Vaidya, S (2014). "Spectrum of ovarian tumors in a referral hospital in Nepal
". Journal of Pathology of Nepal 4 (7): 539–543. doi:. ISSN 2091-0908.
- Minor adjustment for mature cystic teratomas (0.17 to 2% risk of ovarian cancer): Mandal, Shramana; Badhe, Bhawana A. (2012). "Malignant Transformation in a Mature Teratoma with Metastatic Deposits in the Omentum: A Case Report ". Case Reports in Pathology 2012: 1–3. doi:. ISSN 2090-6781. - ↑ 2.0 2.1 2.2 2.3 Unless otherwise specified in boxes, reference is: Vaidya, SA; Kc, S; Sharma, P; Vaidya, S (2014). "Spectrum of ovarian tumors in a referral hospital in Nepal ". Journal of Pathology of Nepal 4 (7): 539–543. doi:. ISSN 2091-0908.
- ↑ Hillary Rose Elwood. Skin nonmelanocytic tumor - Other tumors of skin - Benign (mature) cystic teratoma. pathology Outlines. Topic Completed: 1 November 2016. Revised: 4 April 2019
- ↑ Sun, Hang; Ding, Hongxin; Wang, Jianjun; Zhang, Emma; Fang, Yihua; Li, Zhenhua; Yu, Xiao; Wang, Chongren; et al. (2019). "The differences between gonadal and extra-gonadal malignant teratomas in both genders and the effects of chemotherapy ". BMC Cancer 19 (1). doi:. ISSN 1471-2407.
- ↑ Fischerova D, Indrielle-Kelly T, Burgetova A, Bennett RJ, Gregova M, Dundr P (2022). "Yolk Sac Tumor of the Omentum: A Case Report and Literature Review.
". Diagnostics (Basel) 12 (2). doi:. PMID 35204394. PMC: 8871053. Archived from the original. .
- "This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/)." - ↑ 6.0 6.1 Baradwan, Saeed; Alalyani, Haneen; Baradwan, Amira; Baradwan, Afnan; Al-Ghamdi, Maram; Alnemari, Jameel; Al-Jaroudi, Dania (2018). "Bilateral ovarian masses with different histopathology in each ovary ". Clinical Case Reports 6 (5): 784–787. doi:. ISSN 20500904.
- ↑ Shahrzad Ehdaivand. Ovary tumor - Endometrioid tumors - General. Pathology Outlines. Topic Completed: 1 December 2012. Revised: 6 March 2020
- ↑ Parwate, Nikhil Sadanand; Patel, Shilpa M.; Arora, Ruchi; Gupta, Monisha (2015). "Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature ". The Journal of Obstetrics and Gynecology of India 66 (6): 460–465. doi:. ISSN 0971-9202.
- ↑ Shahrzad Ehdaivand. Ovary tumor - Sex cord stromal tumors - Granulosa cell tumor - adult. Pathology Outlines. Topic Completed: 1 December 2012. Revised: 9 March 2020
- ↑ Schubert TE, Stoehr R, Hartmann A, Schöne S, Löbelenz M, Mikuz G (2014). "Adult type granulosa cell tumor of the testis with a heterologous sarcomatous component: case report and review of the literature.
". Diagn Pathol 9: 107. doi:. PMID 24894598. PMC: 4100032. Archived from the original. . - Figure 2
- "This article is licensed under a Creative Commons Attribution 4.0 International License" - ↑ 11.0 11.1 11.2 Zhengshan Chen, M.D., Ph.D., Manju Aron, M.D.. Testis & epididymis - Sex cord-stromal tumors - Leydig cell tumor. PathologyOutlines. Topic Completed: 4 March 2021. Minor changes: 12 April 2021.
- ↑ Lisa Lee-Jones, University of Wales College of Medicine (2003-12-01). Ovarian tumours : an overview. Atlas of Genetics and Cytogenetics in Oncology and Haematology.
- ↑ Nicole Riddle, M.D., Jamie Shutter, M.D.. Fallopian tubes & broad ligament - Broad ligament - Mesonephric duct remnants. Pathology Outlines. Topic Completed: 1 May 2013. Minor changes: 30 December 2020
- ↑ Amin, Mahul (2017). AJCC cancer staging manual
(8 ed.). Switzerland: Springer. ISBN 978-3-319-40617-6. OCLC 961218414.
- For access, see the Secrets chapter of Patholines.
- Copyright note: The AJCC, 8th Ed. is published by a company in Switzerland, and the tables presented therein are Public Domain because they consist of tabular information without literary or artistic innovation, and therefore do not fulfil the inclusion criterion of the Swiss Copyright Act (CopA) which applies to "literary and artistic intellectual creations with individual character" (see Federal Act on Copyright and Related Rights (Copyright Act, CopA) of 9 October 1992 (Status as of 1 January 2022)).
Image sources



