Cervical cytology
Author:
Mikael Häggström [note 1]
Cytology of the cervix:
Contents
Clinical information
It is not necessary to look through more than readily available reports from previous cervical cytologies.
Magnification
While being fairly new to cervical cytology, preferably start looking at a high magnification such as 20x objective (with 10x eye piece). For suspicious findings, you may magnify up to maximum. On the other hand, once the pattern feels repetitive you can try switching to a slightly lower magnification such as 10x.
Adequacy
Adequacy should always be stated, either as "Satisfactory" or "Unsatisfactory". For estimating the number of cells, determine the following:
- The area of your field of view at high power (see the Evaluation chapter)
- The total size of the relevant area on the microscope slide. A ThinPrep is about 360 mm2.
- Look at 10 representative high power fields (HPFs) within that area, and calculate the average number of cells per high power field.
You may count 10 fields either across the slide, or 5 fields in each direction.[1]
| Total number of cells = Average number of cells per HPF * | Total size of area HPF area |
Conventional smear cellularity should be at least 8,000 cells. Liquid-based cytology cellularity should be at least 5,000 cells. Also a conventional smear is inadequate if >75% of cells are obscured by blood, exudate or air-drying artefact.[1]
Eventually you will be able to tell when most cases are adequate or inadequate without performing a detailed calculation.
Transformation zone presence
State whether the endocervical/transformation zone is present or absent. Count an endocervical component as present if there are 10 or more endocervical or squamous metaplastic cells.[2]
In patients with previous hysterectomy, simply report glandular or squamous metaplastic cells as such, rather than stating the presence of a transformation zone, since they are likely vaginal in origin in such patients.[3]
Very common findings
Vaginal squamous cell with normal vaginal flora versus bacterial vaginosis on Pap stain. Normal vaginal flora (left) is predominantly rod-shaped Lactobacilli, whereas in bacterial vaginosis (right) there are clue cells, covered in bacteria. A significant amount of clue cells can be reported as "Shift in vaginal flora suggestive of bacterial vaginosis".
Main conditions to exclude or confirm
Squamous atypia, seen mainly as cells with increased nucleus/cytoplasm ratio, nuclear hyperchromasia and irregular nuclear outline.
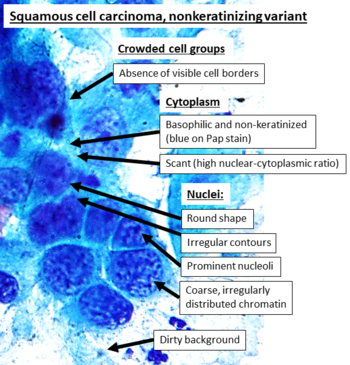
Cytopathology of squamous cell carcinoma, keratinizing variant, with typical features.[4] Pap stain.
Clinical implication
If you are uncertain of the degree of dysplasia, it can be useful to look up how much difference it will likely make for the management of the patient. You may make an Internet search for the management of abnormal cervical screening in your region (such as The ASCCP tool for management in the US). A change from close follow-up to colposcopy is not that big of a deal, but if one of the alternatives will lead to a diagnostic excision, make sure that the case is looked upon by commensurate expertise.
Other findings
Report
Example in a normal case:
Cervical/endocervical ThinPrep:
|
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
Main page
References
- ↑ 1.0 1.1 . Criteria for adequacy of a cervical cytology sample. EuroCytology. Retrieved on 2022-08-29.
- ↑ Cibas, Edmund S.; Ducatman, Barbara S. (2021). Cytology : diagnostic principles and clinical correlates . Philadelphia, PA. p. 9. ISBN 978-0-323-63637-7. OCLC 1138033641.
- ↑ Ramirez NC, Sastry LK, Pisharodi LR (2000). "Benign glandular and squamous metaplastic-like cells seen in vaginal Pap smears of post hysterectomy patients: incidence and patient profile. ". Eur J Gynaecol Oncol 21 (1): 43-8. PMID 10726617. Archived from the original. .
- ↑ - Image annotated by Mikael Häggström
- Reference for entries: Gulisa Turashvili, M.D., Ph.D.. Cervix - Squamous cell carcinoma and variants. Pathology Outlines. Last author update: 24 September 2020. Last staff update: 4 April 2022.
- Source image from National Cancer Institute (Public Domain) - ↑ - Image annotated by Mikael Häggström
- Reference for entries: Gulisa Turashvili, M.D., Ph.D.. Cervix - Squamous cell carcinoma and variants. Pathology Outlines. Last author update: 24 September 2020. Last staff update: 4 April 2022.
- Source image by Ravi Mehrotra, Anurag Gupta, Mamta Singh and Rahela Ibrahim (Creative Commons Attribution 2.0 Generic license.) - ↑ Alrajjal A, Pansare V, Choudhury MSR, Khan MYA, Shidham VB (2021). "Squamous intraepithelial lesions (SIL: LSIL, HSIL, ASCUS, ASC-H, LSIL-H) of Uterine Cervix and Bethesda System. ". Cytojournal 18: 16. doi:. PMID 34345247. PMC: 8326095. Archived from the original. .
- ↑ Authors: Caroline I.M. Underwood, M.D., Alexis Musick, B.S., Carolyn Glass, M.D., Ph.D.. Adenocarcinoma overview. Pathology Outlines. Last staff update: 19 July 2022
Image sources














