Dermal nevus
Author:
Mikael Häggström [note 1]
A suspected dermal (or intradermal nevus) generally presents as a dark skin focality.
Contents
Gross processing of skin excisions
| Lesion size | |||
|---|---|---|---|
| <4 mm | 4 - 8 mm | 9 - 15 mm | |
| Benign appearance | |||
| Suspected malignancy | 
|

|
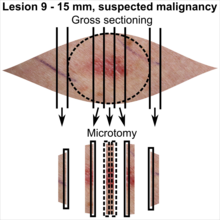
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Comprehensiveness
On this resource, the following formatting is used for comprehensiveness:
- Minimal depth
- (Moderate depth)
- ((Comprehensive))
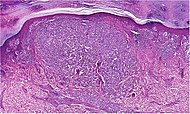
Microscopic evaluation
- Irregularly distributed dermal nests of melanocytes.[2]
- Atypia
A dermal nevus infrequently shows multinucleated giant cells as shown.[3]
Subtyping
Differential diagnosis
Mainly:
Junctional nevus (here seen in H&E stain and Melan A stain), where all nests are continuous with the epidermis.
Invasive melanoma of the skin, has more atypia and dysplasia (see table in the grading section).
Grading
(Grade a dermal nevus into either low or high grade by the following algorithm:)[4]
In uncertain cases,(( more specific grading,)) and/or differentiation from a non-atypical congenital nevus and suspected invasive melanoma, the following table can be used to determine the most fitting diagnosis:
| Parameter | Non-dysplastic dermal nevus | Low-grade dysplastic dermal nevus | High-grade dysplastic dermal nevus | Suspected invasive melanoma | ||
|---|---|---|---|---|---|---|
| Mild dysplasia | Moderate dysplasia | Severe dysplasia | ||||
| Macroscopic | Lateral circumscription[5] | Sharp | Slightly diminished | Moderate | Poor | |
| Symmetry[5] | Good | Often broken | Rare | |||
| Structural (Low mag.) |
Micrograph |  |
| |||
| Delimitation[2] | Rarely diffuse | Sometimes diffuse | Often diffuse | |||
| Confluent nests[2] | Rarely | Sometimes | Often | Often widespread | ||
| Pigment distribution[2] | Regular | Irregular | ||||
| Concentric fibrosis | Regressive (see below table)[5] | Yes[2] | Occasional[5] | |||
| Lamellar fibrosis | Rarely[2] | Often[2] | Often pronounced[2] | Occasional[5] | ||
| Lymphocytic infiltrate[2] | Mild, perivascular | Mild or moderate, perivascular | Varying | Varying | ||
| Cellular (high mag.) |
Micrographs | 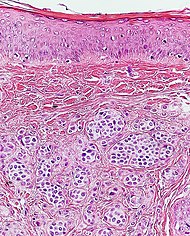 |

| |||
| Nuclear size[5] | Small | Medium | Large | Medium or large. Pleomorphic[6] | ||
| Nuclear pleomorphism[7] | Slight superficial | Slight | Prominent | |||
| Chromatin pattern | Uniform[5] | Condensed[5] | Partically expanded[5] | Expanded, coarse in some cells[5] | Expanded, hyperchromatic, coarse.[5] Usually granular.[7] | |
| Nucleoli[5] | Small | Medium | Large | Usually[7] large | ||
| Mitoses[5] | Few superficial | Superficial and deep | ||||
| Histological regression[7] (see below table) | Usually | Usually not | ||||
| Percentage of atypical melanocytes[2] | <10% | About 10 - 50% | about 50-90% | Usually> 90% | ||
Histological regression is one or more areas within a tumor in which neoplastic cells have disappeared or decreased in number. In this case, it means complete or partial disappearance of neoplastic cells from areas of the dermis (and occasionally from the epidermis), which have been replaced by fibrosis, accompanied by melanophages, new blood vessels, and a variable degree of inflammation.[8]
In suspected but not certain nevus or melanoma, generally perform immunohistochemistry with SOX10 (which stains cell nuclei of melanocytes), whereby melanocyte proliferation and nuclear pleomorphism is easier to see:[9]
Report
- Diagnosis of dermal nevus.
- (Most likely grade.)
Example:
| (Skin, right upper chest, shave biopsy:) Intradermal (low-grade) nevus. |
See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ The excision examples show a normal mole (upper row, benign appearance) and a superficial basal cell carcinoma (lower row, suspected malignancy).
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the tips to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each tip. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Katarzyna Lundmark, Britta Krynitz, Ismini Vassilaki, Lena Mölne, Annika Ternesten Bratel. Histopatologisk bedömning och gradering av dysplastiskt nevus samt gränsdragning mot melanom in situ/melanom (Histopathological assessment and grading of dysplastic nevus and distinction from melanoma in situ/melanoma). KVAST (Swedish Society of Pathology). Retrieved on 2019-09-18.
- ↑ Christopher S. Hale, M.D.. Skin melanocytic tumor - Dermal nevus. PathologyOutlines. Topic Completed: 1 August 2014. Minor changes: 21 September 2020
- ↑ Pozo, Lucia; Naase, Mahmoud; Cerio, Rino; Blanes, Alfredo; Diaz-Cano, Salvador J. (2001). "Critical Analysis of Histologic Criteria for Grading Atypical (Dysplastic) Melanocytic Nevi ". American Journal of Clinical Pathology 115 (2): 194–204. doi:. ISSN 0002-9173.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Arumi-Uria, Montserrat; McNutt, N Scott; Finnerty, Bridget (2003). "Grading of Atypia in Nevi: Correlation with Melanoma Risk ". Modern Pathology 16 (8): 764–771. doi:. ISSN 0893-3952.
- ↑ Christopher S. Hale. Skin melanocytic tumor - Melanoma - Invasive melanoma. Topic Completed: 1 May 2013. Revised: 17 September 2019
- ↑ 7.0 7.1 7.2 7.3 Husain, Ehab A; Mein, Charles; Pozo, Lucia; Blanes, Alfredo; Diaz-Cano, Salvador J (2011). "Heterogeneous topographic profiles of kinetic and cell cycle regulator microsatellites in atypical (dysplastic) melanocytic nevi ". Modern Pathology 24 (4): 471–486. doi:. ISSN 0893-3952.
- ↑ Ribero, Simone; Gualano, Maria Rosaria; Osella-Abate, Simona; Scaioli, Giacomo; Bert, Fabrizio; Sanlorenzo, Martina; Balagna, Elena; Fierro, Maria Teresa; et al. (2015). "Association of Histologic Regression in Primary Melanoma With Sentinel Lymph Node Status ". JAMA Dermatology 151 (12): 1301. doi:. ISSN 2168-6068.
- ↑ Miettinen, Markku; McCue, Peter A.; Sarlomo-Rikala, Maarit; Biernat, Wojciech; Czapiewski, Piotr; Kopczynski, Janusz; Thompson, Lester D.; Lasota, Jerzy; et al. (2015). "Sox10—A Marker for Not Only Schwannian and Melanocytic Neoplasms But Also Myoepithelial Cell Tumors of Soft Tissue ". The American Journal of Surgical Pathology 39 (6): 826–835. doi:. ISSN 0147-5185.
Image sources












