Invasive melanoma of the skin
Author:
Mikael Häggström [note 1]
Melanoma of the skin generally presents as a dark skin focality.
Contents
Fixation
Generally 10% neutral buffered formalin.
See also: General notes on fixation
Gross processing
Gross examination
Note:
- Color
- Well-defined or diffuse border
- Size
- Any elevation
Tissue selection
| <4 mm | 4 - 8 mm | 9 - 15 mm |
|---|---|---|

|

|
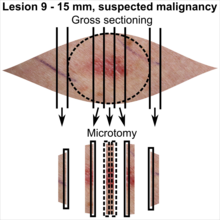
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Microscopic evaluation
Differential diagnoses
Melanoma in situ, where melanoma cells are limited to the epidermis.[2]
Dermal nevus
| Parameter | Non-dysplastic dermal nevus | Low-grade dysplastic dermal nevus | High-grade dysplastic dermal nevus | Suspected invasive melanoma | ||
|---|---|---|---|---|---|---|
| Mild dysplasia | Moderate dysplasia | Severe dysplasia | ||||
| Macroscopic | Lateral circumscription[3] | Sharp | Slightly diminished | Moderate | Poor | |
| Symmetry[3] | Good | Often broken | Rare | |||
| Structural (Low mag.) |
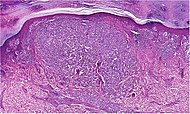
Micrograph |  |
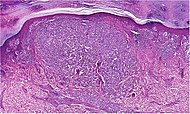
| |||
| Delimitation[4] | Rarely diffuse | Sometimes diffuse | Often diffuse | |||
| Confluent nests[4] | Rarely | Sometimes | Often | Often widespread | ||
| Pigment distribution[4] | Regular | Irregular | ||||
| Concentric fibrosis | Regressive (see below table)[3] | Yes[4] | Occasional[3] | |||
| Lamellar fibrosis | Rarely[4] | Often[4] | Often pronounced[4] | Occasional[3] | ||
| Lymphocytic infiltrate[4] | Mild, perivascular | Mild or moderate, perivascular | Varying | Varying | ||
| Cellular (high mag.) |
Micrographs | 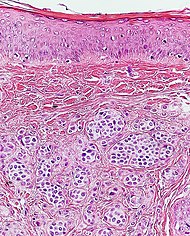 |

| |||
| Nuclear size[3] | Small | Medium | Large | Medium or large. Pleomorphic[5] | ||
| Nuclear pleomorphism[6] | Slight superficial | Slight | Prominent | |||
| Chromatin pattern | Uniform[3] | Condensed[3] | Partically expanded[3] | Expanded, coarse in some cells[3] | Expanded, hyperchromatic, coarse.[3] Usually granular.[6] | |
| Nucleoli[3] | Small | Medium | Large | Usually[6] large | ||
| Mitoses[3] | Few superficial | Superficial and deep | ||||
| Histological regression[6] (see below table) | Usually | Usually not | ||||
| Percentage of atypical melanocytes[4] | <10% | About 10 - 50% | about 50-90% | Usually> 90% | ||
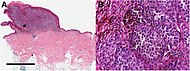
Histological regression is one or more areas within a tumor in which neoplastic cells have disappeared or decreased in number. In this case, it means complete or partial disappearance of neoplastic cells from areas of the dermis (and occasionally from the epidermis), which have been replaced by fibrosis, accompanied by melanophages, new blood vessels, and a variable degree of inflammation.[7]
In suspected but not certain nevus or melanoma, generally perform immunohistochemistry with SOX10 (which stains cell nuclei of melanocytes), whereby melanocyte proliferation and nuclear pleomorphism is easier to see:[8]
Further workup
In case a diagnosis of invasive melanoma of the skin can be made, the following are generally mandatory:
- Margins
- Depth
- Any ulceration
- Histopathologic type.[9]
- Presence of mitoses in the intradermal component.[9]
The following aspects are mandatory in some regions:
- Clark's level (not mandatory in the US)[note 3]
Margins
Determine if the distance to any margin is greater or lesser than 3 mm.[10] If a margin is closer, measure it at an exactness of 0.1 mm.
If margins are difficult to determine, consider immunohistochemistry with SOX10 (staining the nuclei of melanocytes), to better visualize melanoma nests.[11]
Depth and ulceration
For invasive melanoma, measure the depth and whether there is ulceration or not, so as to be able to classify the T stage (following table by AJCC, 8th edition):[12]
| T Category | Thickness | Ulceration status |
|---|---|---|
| TX: primary tumor thickness cannot be assessed (e.g., diagnosis by curettage) |
Not applicable | Not applicable |
| T0: no evidence of primary tumor (e.g., unknown primary or completely regressed melanoma) |
Not applicable | Not applicable |
| Tis (melanoma in situ) | Not applicable | Not applicable |
| T1 | ≤1.0 mm | Unknown or unspecified |
| T1a | <0.8 mm | Without ulceration |
| T1b | <0.8 mm | With ulceration |
| 0.8–1.0 mm | With or without ulceration | |
| T2 | >1.0–2.0 mm | Unknown or unspecified |
| T2a | >1.0–2.0 mm | Without ulceration |
| T2b | >1.0–2.0 mm | With ulceration |
| T3 | >2.0‐4.0 mm | Unknown or unspecified |
| T3a | >2.0–4.0 mm | Without ulceration |
| T3b | >2.0–4.0 mm | With ulceration |
| T4 | >4.0 mm | Unknown or unspecified |
| T4a | >4.0 mm | Without ulceration |
| T4b | >4.0 mm | With ulceration |
Histopathologic type
If needing to evaluate, the main types of invasive melanoma are:[13]
| Type | Features | Relative incidence (in comparison to all melanomas)[13] |
Photograph | Micrograph |
|---|---|---|---|---|
| Superficial spreading melanoma | Melanoma cells with nest formation along the dermo-epidermal junction. | 70% | 
|

|
| Nodular melanoma | Grows relatively more in depth than in width. | 15% - 20% | 
|
|
| Lentigo maligna melanoma | Atypical epidermal melanocytes as well as invasion into the dermis.[14] | 5% - 10% | 
|

|
| Acral lentiginous melanoma | Continuous proliferation of atypical melanocytes at the dermoepidermal junction.[15] | 7% - 10% | 
|
|
Clark's level
If needing to evaluate,[note 3] Clark's levels are:[16]
- Level 1: Melanoma confined to the epidermis (melanoma in situ)
- Level 2: Invasion into the papillary dermis
- Level 3: Invasion to the junction of the papillary and reticular dermis
- Level 4: Invasion into the reticular dermis
- Level 5: Invasion into subcutaneous tissue.
Tumor‐infiltrating Lymphocytes (TILs)
Classify as either of the following:[12]
- Absent TIL infiltrate: no lymphocytes present or, if present, they do not interact with tumor cells.
- Non-brisk TIL infiltrate: focal areas of lymphocytic infiltration in the tumor.
- Brisk TIL infiltrate: TIL infiltration of the entire base of the tumor, or diffuse permeation of the tumor.
Lymph nodes

If negative on H&E stain, generally use immunohistochemistry for melanoma markers (such as a combination of melan-A and HMB-45) to exclude micrometastasis:
Other parameters
Optionally, the following parameters can be given:[17]
- histological regression, with complete or partial disappearance from areas of the dermis (and occasionally from the epidermis), which have been replaced by fibrosis, accompanied by melanophages, new blood vessels, and a variable degree of inflammation.[18]
- Further information: Evaluation of tumors
Report
Report when evaluated (as per mandatory vs. optional in Further workup above):
- >3 mm : "Clear margins" (or: "Clear margins at over __ mm")((or the exact distance thereof)).))
- <3 mm but not continuous with edge: "Close margins at __ mm at (location). [[Locations are mainly the deep edge, or the (superior/inferior/medial/lateral) radial edge.]]." Numbers are generally given at an exactness of 0.1 mm.
- Continuous with margin: "Not radically excised at (location)."
- Depth or most distant invasion of melanoma cells.[19]
- Ulceration or not, and maximum dimension if present
- Stage as per AJCC
- Clark's level
- Histopathologic type
- Mitotic rate, as amount per mm2
- Significant signs of regression
- Cytoplasmic pigmentation
- Melanoma cell shapes
US example
|
Skin, mid upper back, excision:
See synoptic report. SYNOPTIC REPORT: Specimen Procedure: Excision Specimen Laterality: Midline Tumor Tumor Site: Skin of trunk Histologic Type: Nodular melanoma Maximum Tumor (Breslow) Thickness (Millimeters): 10 mm Macroscopic Satellite Nodule(s): Not identified Ulceration: Present Extent of Ulceration (Millimeters): 12 mm Anatomic (Clark) Level: IV (Melanoma invades reticular dermis) Mitotic Rate: 18 mitoses / mm2 Microsatellite(s): Not identified Lymphovascular Invasion: Not identified Neurotropism: Not identified Tumor-Infiltrating Lymphocytes: Present, nonbrisk Tumor Regression: Not identified Margins Peripheral Margins: Negative for invasive melanoma Distance of Invasive Melanoma from Closest Peripheral Margin (Millimeters): 5 mm Location: 3 o'clock and 9 o'clock Status of melanoma in situ at peripheral margins: Negative for melanoma in situ Distance of melanoma in situ from closest peripheral margin (millimeters): Cannot be determined - Ulcerated surface and no in-situ noted in the remaining surface Location: Lateral Deep Margin: Negative for invasive melanoma Distance of Invasive Melanoma from Deep Margin (Millimeters): 2 mm Status of Melanoma in situ at Deep Margin: Negative for melanoma in situ Distance of Melanoma in situ from Deep Margin (Millimeters): Cannot be determined (negative for melanoma in situ) Lymph Nodes Regional Lymph Nodes: No lymph nodes submitted or found Pathologic Stage Classification (pTNM, AJCC 8th Edition) Primary Tumor (pT): pT4b Regional Lymph Nodes (pN): pNX |
European example
|
Sun-damaged skin with central diffusely delimited proliferation of melanocytic cells having polymorphic cell nuclei, distinct nucleoli and uneven light brown pigmentation. An area of pagetoid migration is seen. There is ulceration of a smaller area. The radial margin is over 3.0 mm and the deep margin is 2.0 mm.
|
See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ The excision example shows a superficial basal cell carcinoma.
- ↑ 3.0 3.1 Clark's level is not included in United States AJCC guidelines, but is mandatory for melanomas in Sweden.
-. Breslow Depth and Clark Level. Melanoma Research Alliance. Retrieved on 2020-02-13.
- . Bilaga 6. Kvalitetsbilaga för patologi (KVAST-bilaga). Regionala Cancercentrum i Samverkan, guidelines by Swedish Society of Pathology. Retrieved on 2020-02-13.
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the pointy ends to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each pointy end. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- ↑ . Melanoma in situ (stage 0). Cancer Research UK. Last reviewed: 27 Jun 2019
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Arumi-Uria, Montserrat; McNutt, N Scott; Finnerty, Bridget (2003). "Grading of Atypia in Nevi: Correlation with Melanoma Risk ". Modern Pathology 16 (8): 764–771. doi:. ISSN 0893-3952.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Katarzyna Lundmark, Britta Krynitz, Ismini Vassilaki, Lena Mölne, Annika Ternesten Bratel. Histopatologisk bedömning och gradering av dysplastiskt nevus samt gränsdragning mot melanom in situ/melanom (Histopathological assessment and grading of dysplastic nevus and distinction from melanoma in situ/melanoma). KVAST (Swedish Society of Pathology). Retrieved on 2019-09-18.
- ↑ Christopher S. Hale. Skin melanocytic tumor - Melanoma - Invasive melanoma. Topic Completed: 1 May 2013. Revised: 17 September 2019
- ↑ 6.0 6.1 6.2 6.3 Husain, Ehab A; Mein, Charles; Pozo, Lucia; Blanes, Alfredo; Diaz-Cano, Salvador J (2011). "Heterogeneous topographic profiles of kinetic and cell cycle regulator microsatellites in atypical (dysplastic) melanocytic nevi ". Modern Pathology 24 (4): 471–486. doi:. ISSN 0893-3952.
- ↑ Ribero, Simone; Gualano, Maria Rosaria; Osella-Abate, Simona; Scaioli, Giacomo; Bert, Fabrizio; Sanlorenzo, Martina; Balagna, Elena; Fierro, Maria Teresa; et al. (2015). "Association of Histologic Regression in Primary Melanoma With Sentinel Lymph Node Status ". JAMA Dermatology 151 (12): 1301. doi:. ISSN 2168-6068.
- ↑ Miettinen, Markku; McCue, Peter A.; Sarlomo-Rikala, Maarit; Biernat, Wojciech; Czapiewski, Piotr; Kopczynski, Janusz; Thompson, Lester D.; Lasota, Jerzy; et al. (2015). "Sox10—A Marker for Not Only Schwannian and Melanocytic Neoplasms But Also Myoepithelial Cell Tumors of Soft Tissue ". The American Journal of Surgical Pathology 39 (6): 826–835. doi:. ISSN 0147-5185.
- ↑ 9.0 9.1 - USA: . [https://documents.cap.org/protocols/Skin.Melanoma_4.3.0.2.REL_CAPCP.pdf Protocol for the Examination of Excision Specimens From
Patients With Melanoma of the Skin]. COllege of American Pathologists. Version: 4.3.0.2. Protocol Posting Date: November 2021
-Sweden: . Bilaga 6. Kvalitetsbilaga för patologi (KVAST-bilaga). Regionala Cancercentrum i Samverkan, guidelines by Swedish Society of Pathology. Retrieved on 2020-02-13. - ↑ Definition of "thin margin": Wolf, Y.; Balicer, R.D.; Amir, A.; Feinmesser, M.; Hauben, D.J. (2001). "The vertical dimension in the surgical treatment of cutaneous malignant melanoma – how deep is deep? ". European Journal of Plastic Surgery 24 (2): 74–77. doi:. ISSN 0930-343X.
- ↑ Miettinen, Markku; McCue, Peter A.; Sarlomo-Rikala, Maarit; Biernat, Wojciech; Czapiewski, Piotr; Kopczynski, Janusz; Thompson, Lester D.; Lasota, Jerzy; et al. (2015). "Sox10—A Marker for Not Only Schwannian and Melanocytic Neoplasms But Also Myoepithelial Cell Tumors of Soft Tissue ". The American Journal of Surgical Pathology 39 (6): 826–835. doi:. ISSN 0147-5185.
- ↑ 12.0 12.1 Amin, Mahul (2017). AJCC cancer staging manual
(8 ed.). Switzerland: Springer. ISBN 978-3-319-40617-6. OCLC 961218414.
- For access, see the Secrets chapter of Patholines.
- Copyright note: The AJCC, 8th Ed. is published by a company in Switzerland, and the tables presented therein are Public Domain because they consist of tabular information without literary or artistic innovation, and therefore do not fulfil the inclusion criterion of the Swiss Copyright Act (CopA) which applies to "literary and artistic intellectual creations with individual character" (see Federal Act on Copyright and Related Rights (Copyright Act, CopA) of 9 October 1992 (Status as of 1 January 2022)). - ↑ 13.0 13.1 [https://books.google.se/books?id=wGclDwAAQBAJ&pg=PA805 Page 805 in: Ferri, Fred (2019). Ferri's clinical advisor 2019 : 5 books in 1 . Philadelphia, PA: Elsevier. ISBN 978-0-323-52957-0. OCLC 1040695302.
- ↑ Michael Xiong; Ahmad Charifa; Chih Shan J. Chen.. Cancer, Lentigo Maligna Melanoma. StatPearls, National Center for Biotechnology Information. Last Update: May 18, 2019.
- ↑ Piliang, Melissa Peck (2009). "Acral Lentiginous Melanoma ". Surgical Pathology Clinics 2 (3): 535–541. doi:. ISSN 18759181.
- ↑ . NCI Dictionary of Cancer Terms. National Cancer Institute. Retrieved on 2020-02-13.
- ↑ Rees, Jonathan; Viros, Amaya; Fridlyand, Jane; Bauer, Juergen; Lasithiotakis, Konstantin; Garbe, Claus; Pinkel, Daniel; Bastian, Boris C (2008). "Improving Melanoma Classification by Integrating Genetic and Morphologic Features ". PLoS Medicine 5 (6): e120. doi:. ISSN 1549-1676.
- ↑ Ribero, Simone; Gualano, Maria Rosaria; Osella-Abate, Simona; Scaioli, Giacomo; Bert, Fabrizio; Sanlorenzo, Martina; Balagna, Elena; Fierro, Maria Teresa; et al. (2015). "Association of Histologic Regression in Primary Melanoma With Sentinel Lymph Node Status ". JAMA Dermatology 151 (12): 1301. doi:. ISSN 2168-6068.
- ↑ 19.0 19.1 19.2 . An Example of a Melanoma Pathology Report. Melanoma Foundation. Retrieved on 2019-09-24.
Image sources






