Melanoma in situ
Author:
Mikael Häggström [note 1]
Melanoma of the skin generally presents as a dark skin focality and/or a suspected malignant skin excision.
Contents
Fixation
Generally 10% neutral buffered formalin.
See also: General notes on fixation
Gross processing
Gross examination
Note:
- Color
- Well-defined or diffuse border
- Size
- Any elevation
Tissue selection
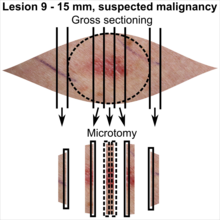
| <4 mm | 4 - 8 mm | 9 - 15 mm |
|---|---|---|

|

|
|
In table above, each top image shows recommended lines for cutting out slices to be submitted for further processing. Bottom image shows which side of the slice that should be put to microtomy. Dashed lines here mean that either side could be used. Further information: Gross processing of skin excisions
Microscopic evaluation
Differential diagnoses
Distinguish mainly from dysplastic nevus and invasive melanoma of the skin:
Dysplastic nevus
| Parameter | Non-atypical congenital pattern | Low-grade dysplastic nevus | High-grade dysplastic nevus | Suspected melanoma in situ | ||
|---|---|---|---|---|---|---|
| Mild dysplasia | Moderate dysplasia | Severe dysplasia | ||||
| Macroscopic | Lateral circumscription[2] | Sharp | Slightly diminished | Moderate | Poor | |
| Symmetry[2] | Good | Often broken | Rare | |||
| Structural (Low mag.) |
Delimitation[3] | Rarely diffuse | Sometimes diffuse | Often diffuse | ||
| Lentiginous proliferation[note 3][3] | Yes, along with rete pegs | Yes, along with and focally between rete pegs | Yes, along with and focally between rete pegs | Yes partially continuous, multilayered | ||
| Bridging[3] | Rarely | Often | ||||
| Confluent nests[3] | Rarely | Sometimes | Often | Often widespread | ||
| Pigment distribution[3] | Regular | Irregular | ||||
| Suprabasal presence (less than most superficial third of subcorneal epidermis) | Occasionally centrally[2] | No[3] or rarely[2] | Occasionally centrally[2] | Yes, multifocal[3] | ||
| Pagetoid migration including superficial third of subcorneal epidermis[3] | No | No | Yes, in a maximum of 2 HPF centrally, but not peripherally | Yes, multifocal and/or in periphery | ||
| Extended rete pegs | Ocassional[2] | Yes, regular[3] | Yes, varying[3] | Yes, often irregular[3] | Varying, flattened[3] | |
| Concentric fibrosis | Regressive[2] | Yes[3] | Occasional[2] | |||
| Lamellar fibrosis | Rarely[3] | Often[3] | Often pronounced[3] | Occasional[2] | ||
| Lymphocytic infiltrate[3] | Mild, perivascular | Mild or moderate, perivascular | Varying | Varying | ||
| Suprapapillary plate involvement | No[2] | Usually no[2] | Often[2] | Yes[2] | ||
| Cellular (high mag.) |
Image |  |
||||
| Junctional extension[2] | Unusual | Usual | Extensive | |||
| Nuclear size[2] | Age-related | Small | Medium | Large | Medium or large. Pleomorphic[4] | |
| Nuclear pleomorphism[5] | Slight | Prominent | ||||
| Chromatin pattern | Uniform[2] | Condensed[2] | Partically expanded[2] | Expanded, coarse in some cells[2] | Expanded, hyperchromatic, coarse.[2] Usually granular.[5] | |
| Nucleoli[2] | Age-related | Small | Medium | Large | Usually[5] large | |
| Mitoses[2] | Few superficial | Superficial and deep | ||||
| Histological regression[5][note 4] | Usually | Usually not | ||||
| Percentage of atypical melanocytes[3] | <10% | About 10 - 50% | about 50-90% | Usually> 90% | ||
| Intradermal melanocytic atypia[3] | No | Rarely, in superficial part | Can be detected in superficial part | |||
| Intradermal melanocyte maturation[3] | Yes | Yes, can be partial | Yes, can be partial | Variable | ||
In suspected but not certain nevus or melanoma in situ, generally perform immunohistochemistry with SOX10, whereby melanocyte proliferation and nuclear pleomorphism is easier to see.[note 5]
- Further information: Evaluation of suspected malignancies
Invasive melanoma of the skin
Invasive melanoma of the skin has features melanoma in situ, but also has dermal involvement of atypical melanocytes with cytologic atypia and no maturation.[6]
Further workup
Upon a diagnosis of melanoma in situ, evaluate its margins.
Optionally, attempt to determine the histopathologic type and amount of cytoplasmic pigmentation:
- Margins
If melanoma, determine if the distance to any margin is greater or lesser than 2-3 mm.
- 2 mm is used as a cutoff for sharply demarcated, small, superficially spreading or nevoid melanomas.[7]
- 3 mm is used for ill-defined lentigo maligna melanoma in situ.[7]
If lesser, quantify the distance.
If margins are difficult to determine, consider immunohistochemistry with SOX10 to better visualize melanoma nests.[note 5]
- Histopathologic type
Main types of melanoma in situ are:
| Type | Features | Micrograph |
|---|---|---|
| Superficial spreading melanoma in situ | Melanoma cells with nest formation along the dermo-epidermal junction. | 
|
| Lentigo maligna | Linear spread of atypical epidermal melanocytes along stratum basale.[8] | |
| Acral lentiginous melanoma in situ | Continuous proliferation of atypical melanocytes at the dermoepidermal junction.[9] | 
|
Report
Most important entries:
- >2 or 3 mm (as per Further workup above): "Clear margins" (or: "Clear margins at over __ mm")((or the exact distance thereof)).))
- <2 or 3 mm but not continuous with edge: "Close margins at __ mm at (location). [[Locations are mainly the deep edge, or the (superior/inferior/medial/lateral) radial edge.]]." Numbers are generally given at an exactness of 0.1 mm.
- Continuous with margin: "Not radically excised at (location)."
See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Patholines:Authorship for details.
- ↑ The excision example shows a superficial basal cell carcinoma.
- ↑ Lentiginous proliferation is proliferation along the basal layer of the epidermis
- ↑ Histological regression is one or more areas within a tumor in which neoplastic cells have disappeared or decreased in number. In this case, this means complete or partial disappearance from areas of the dermis (and occasionally from the epidermis), which have been replaced by fibrosis, accompanied by melanophages, new blood vessels, and a variable degree of inflammation.
- Ribero, Simone; Gualano, Maria Rosaria; Osella-Abate, Simona; Scaioli, Giacomo; Bert, Fabrizio; Sanlorenzo, Martina; Balagna, Elena; Fierro, Maria Teresa; et al. (2015). "Association of Histologic Regression in Primary Melanoma With Sentinel Lymph Node Status ". JAMA Dermatology 151 (12): 1301. doi:. ISSN 2168-6068. - ↑ 5.0 5.1 SOX10 stains cell nuclei of melanocytes.
- Miettinen, Markku; McCue, Peter A.; Sarlomo-Rikala, Maarit; Biernat, Wojciech; Czapiewski, Piotr; Kopczynski, Janusz; Thompson, Lester D.; Lasota, Jerzy; et al. (2015). "Sox10—A Marker for Not Only Schwannian and Melanocytic Neoplasms But Also Myoepithelial Cell Tumors of Soft Tissue ". The American Journal of Surgical Pathology 39 (6): 826–835. doi:. ISSN 0147-5185.
Main page
References
- ↑ There are many variants for the processing of skin excisions. These examples use aspects from the following sources:
- . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- For number of slices and coverage of lesions, depending on size. - Monica Dahlgren, Janne Malina, Anna Måsbäck, Otto Ljungberg. Stora utskärningen. KVAST (Swedish Society of Pathology). Retrieved on 2019-09-26.
- For slices towards the pointy ends to determine radicality, which can be parallel to the slices through the lesions (shown), or as longitudinal slices that go through each pointy end. - . Dermatopathology Grossing Guidelines. University of California, Los Angeles. Retrieved on 2019-10-23.
- For microtomy of the most central side at the lesion - "The principles of mohs micrographic surgery for cutaneous neoplasia
- With a "standard histologic examination" that, in addition to the lesion, only includes one section from each side along the longest diameter of the specimen.
- It also shows an example of circular coverage, with equal coverage distance in all four directions.
- The entire specimen may be submitted if the risk of malignancy is high. - . Handläggning av hudprover – provtagningsanvisningar, utskärningsprinciper och snittning (Handling of skin samples - sampling instructions, cutting principles and incision. Swedish Society of Pathology.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 Arumi-Uria, Montserrat; McNutt, N Scott; Finnerty, Bridget (2003). "Grading of Atypia in Nevi: Correlation with Melanoma Risk ". Modern Pathology 16 (8): 764–771. doi:. ISSN 0893-3952.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 Katarzyna Lundmark, Britta Krynitz, Ismini Vassilaki, Lena Mölne, Annika Ternesten Bratel. Histopatologisk bedömning och gradering av dysplastiskt nevus samt gränsdragning mot melanom in situ/melanom (Histopathological assessment and grading of dysplastic nevus and distinction from melanoma in situ/melanoma). KVAST (Swedish Society of Pathology). Retrieved on 2019-09-18.
- ↑ Christopher S. Hale. Skin melanocytic tumor - Melanoma - Invasive melanoma. Topic Completed: 1 May 2013. Revised: 17 September 2019
- ↑ 5.0 5.1 5.2 5.3 Husain, Ehab A; Mein, Charles; Pozo, Lucia; Blanes, Alfredo; Diaz-Cano, Salvador J (2011). "Heterogeneous topographic profiles of kinetic and cell cycle regulator microsatellites in atypical (dysplastic) melanocytic nevi ". Modern Pathology 24 (4): 471–486. doi:. ISSN 0893-3952.
- ↑ Christopher S. Hale. Skin melanocytic tumor - Melanoma - Invasive melanoma. Pathology Outlines. Topic Completed: 1 May 2013. Revised: 17 September 2019
- ↑ 7.0 7.1 Measurements used to classify a melanoma as radical: Page 406 in: Klaus J. Busam, Richard A Scolyer, Pedram Gerami (2018). Pathology of Melanocytic Tumors . Elsevier Health Sciences. ISBN 9780323508681.
- ↑ Error on call to Template:cite web: Parameters url and title must be specifiedHon A/Prof Amanda Oakley (2011). . DermNet NZ.
- ↑ Piliang, Melissa Peck (2009). "Acral Lentiginous Melanoma ". Surgical Pathology Clinics 2 (3): 535–541. doi:. ISSN 18759181.
- ↑ 10.0 10.1 . An Example of a Melanoma Pathology Report. Melanoma Foundation. Retrieved on 2019-09-24.
Image sources





